The Ultimate Guide to Streamlining Billing with Medical Electronic Claims Submission
In today’s fast-paced healthcare environment, managing billing processes efficiently is crucial. With the ever-growing number of patients, healthcare providers are constantly seeking ways to streamline their billing procedures. Enter medical electronic claims submission–a game changer in the world of medical billing.
Gone are the days of laboriously filling out paper forms and waiting weeks for reimbursement. Medical electronic claims submission not only improve the speed and accuracy of billing but also enhance the overall experience for both healthcare providers and patients. But how exactly does this system work, and why is it so important for modern healthcare?
What is Medical Electronic Claims Submission?
The term “medical electronic claim submission” is the process of submitting health claims electronically to insurance firms or payers. Instead of together the traditional method of paper submission health care providers can submit claims electronically using special software that allows faster processing and reimbursement.
For healthcare professionals medical electronic claims submission greatly reduces the administrative burden. It helps reduce errors made in manual processes, cuts down on the time to pay, and makes sure that claims are promptly processed. In the highly competitive field of healthcare using electronic claims processing is an essential step towards operational efficiency.
Benefits of Medical Electronic Claims Submission
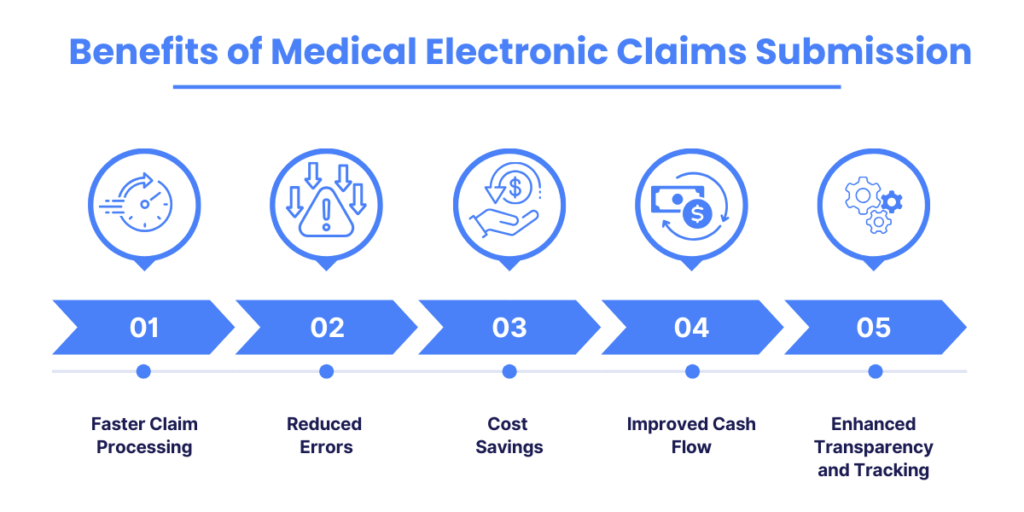
1- Faster Claim Processing
- Automatization and Efficiency: Electronic claims remove the need for manual paperwork, speeding up the process of processing and transmission with automation.
- Real-time Validation: Claims are verified in real-time, which reduces errors and limiting the exchange of information between payers and providers.
- Reduced Data Entry Errors: Built-in validation and prefilled fields reduce mistakes, allowing faster processing.
- Streamlined Communication: Fast and secure transmission of claims will ensure rapid updates and faster payment information between the payer and the provider.
2- Reduced Errors
- Minimum Human Error: Using less manual data entry can reduce common errors such as typos and incorrect calculations.
- Data Validation Checks: Incorrect or incomplete details are immediately flagged to allow for timely corrections and minimizing the requirement for resubmission.
- Standardization: Claim forms follow the standardized codes and formats, which reduces the risk of mistakes caused by misinterpretation or inconsistent information.
- Clear Documentation: Complete and accurate data assures a smooth processing time which reduces errors and improves documentation.
- Improved Error Handling: Real-time flagging for inconsistencies permits immediate resolution, eliminating delays.
3- Cost Savings
- Reduce the need for paper and postage: Electronic submissions eliminate the requirement for paper documents, and also reduce postage costs.
- Eliminate Rejections and Errors: Fewer mistakes and claims rejections can save time and money.
- Improve Accuracy and Comply: Ensuring compliance with the coding standards prevents penalties and can result in cost savings.
- Improve Reporting and Tracking: Better tracking and reporting benefit to identify areas that could be used for cost reduction.
4- Increased Accuracy
- Improve Data Integrity: Electronic submissions minimize manual errors, increasing the accuracy of information on claims.
- Standardize Coding: By enforcing standardized coding, electronic systems ensure accurate claim billing.
- Automated Validation: Automatic validation finds and corrects any errors prior to the submission of claims, ensuring that they are the accuracy and completeness of claims.
- Enable Real-Time Claim Edits: Errors or missing information can be fixed immediately by reducing follow-up messages and increasing the accuracy.
5- Improved Cash Flow
- Payroll Processing Accelerates Accelerate the process of claims made electronically results in faster reimbursements and a better cash flow.
- Reduce the amount of time spent waiting for payments: Electronic submissions streamline adjudication, decreasing delays and making sure that cash flows are steady.
- Provide Prompt Claim Status Updates: Status updates in real-time enable providers to track claim progress and take steps when needed to assure speedier settlements.
- Limit Rejections of Claims: Automated validation checks benefit stop rejections, thereby increasing cash flow.
6- Enhanced Transparency and Tracking
- Enhance Visibility: Digital systems add transparent information about the complete claim processing and submission lifecycle.
- Track claim status: Service providers are able to track claim progress in real time keeping track of the entire process.
- Audit Trail: Electronic records that document the submissions, edits, and revisions assure transparency with a transparent audit trail.
- Enhanced Data Analytics: Data analytics offer insights into claims performance and benefit identify patterns and enhance processes.
7- Streamlined Workflow and Productivity
- Automate Tasks: Automatizing manual tasks increases productivity and speeds up workflow.
- Eliminate Paperwork: The replacement of paper-based documents with electronic systems improves the efficiency.
- Speed up Data Entry: Validation checks and pre-populated fields accelerate data entry, increasing efficiency.
- Centralize Access to Data Access: Centralized access to claim data increases workflow efficiency, removing the need to search manually and increasing overall efficiency.
Conclusion
In conclusion, adopting medical electronic claims submission is a transformative step for enhancing the efficiency and accuracy of billing processes. By leveraging technology to automate and streamline claims, healthcare providers can significantly reduce processing times, minimize errors, and improve cash flow. While challenges such as software integration and data security must be addressed, the benefits—faster reimbursements, reduced administrative burdens, and enhanced accuracy—far outweigh the drawbacks. Embracing electronic claims submission not only optimizes billing practices but also allows healthcare providers to focus more on delivering quality patient care.
Frequently Asked Questions(Faqs)
Electronic claims submission is the process of sending healthcare claims to insurance payers through digital systems rather than using paper forms. This method allows for faster, more accurate processing, reducing errors and improving communication between healthcare providers and payers.
An advantage of electronic claim submission is faster processing. By eliminating manual paperwork and utilizing automated systems, claims are transmitted more quickly, reducing delays and speeding up reimbursements for healthcare providers.
A manual claim submission involves filling out paper forms and mailing them to insurance payers, which can be slow and prone to errors. In contrast, an electronic claim submission uses digital systems to transmit claims directly to payers, leading to faster processing, reduced errors, and more efficient tracking.
Disadvantages of electronic claims include potential software integration issues, which can complicate setup and compatibility with existing systems. Additionally, staff may require extensive training to effectively use the new systems. There are also concerns about data security and compliance with ever-evolving regulations. Finally, technical issues or system downtime can disrupt the claims process and delay submissions.